View list of treatments
View list of treatments for specific diseases
Treating Dry Eye Syndrome and the many related conditions can be frustrating for both doctors and patients. Patients typically want and expect immediate relief from symptoms and doctors usually only have a small arsenal of tools (warm compresses, lid wipes, lubricating drops, topical or oral antibiotics, topical steroids, and lid massage) from which to choose in prescribing treatment. The exception here is the rare, highly skilled physician who specializes in corneal and external diseases, and has had a decades-long practice of treating Dry Eye Syndrome. These doctors have many tools in their arsenals.
The important thing for both doctors and patients to remember is that it is first and foremost critical to diagnose all of the co-morbid diseases, including any systemic ones, and then begin a course of treatment that addresses the most bothersome symptoms first so that the patient can begin to feel relief as quickly as possible. For co-morbid systemic conditions, patients should be referred to their Primary Care Physician or an appropriate specialist.
Even after treatment begins, as patients begin to feel better, it is not uncommon for some new symptoms to crop up or an old symptom to persist. Assuming an accurate diagnosis of the co-morbidities, and targeted treatments specific for each one diagnosed, there are several reasons why a patient may experience new symptoms, or old symptoms may persist.
First, it is very likely that one of the other co-morbid conditions is now being felt by the patient. This may happen because the eyes feel only the most prominent symptom (see Tight Shoes). Once the most prominent symptom is addressed, the next most prominent symptom crops up. Patients may complain that they never had this new symptom until after they started treatment and blame the occurrence of the symptom on the treatment. They may not understand that, in all probability, the new symptom is an indication of a co-morbid condition that was already there, but not felt, because it was not as prominent symptomatically.
Second, even when treated, symptoms may persist because there are co-morbid conditions that present with the exact same symptoms. In this case, the patient may complain that the treatment had no effect; whereas, it is clinically clear that there was a positive outcome.
When new symptoms crop up or symptoms persist, it is crucial that patients continue to communicate with their doctors and let them know how they feel, regardless of how frustrated the patients may feel or if they are losing hope. No doctor can possibly know what new symptom is bothering a patient unless the information is communicated to the doctor with as much precision as possible.
Fundamentally, it is important for everyone involved in treating the patient to understand that the pain and discomfort of Dry Eye is not “in the patient’s head.” There are diagnosable conditions for every symptom and each of these needs to be treated in turn. Patients should also understand that Dry Eye can be a serious condition that may take a long time to get under control, but, with persistence and diligence, it is not impossible.
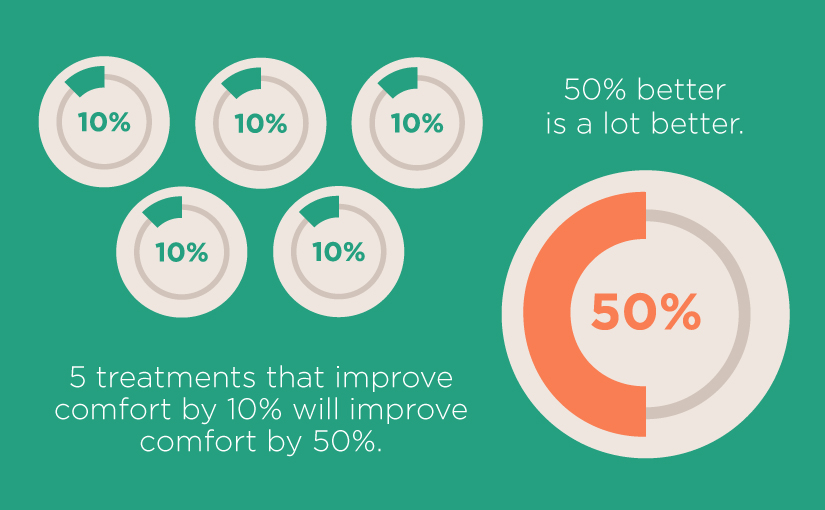
Finally, doctors and patients should also keep in mind that even small improvements can contribute to overall comfort and that many small improvements can lead to even more comfort. In short, every little step that might help to improve comfort, even just a little, should be taken, because every little bit helps. We like to think of this as a simple math problem. One of our doctors explained it like this: if a single treatment improves comfort by 10%, then 5 treatments that improve comfort by 10% will improve overall comfort by 50%. And 50% better is a lot better!
See Clinical Trials for new or experimental treatments.
List of Treatments
Allergy Drops
Amniotic Membrane Transplant (AMT)
Antibiotic Drops and Ointments
Autologous Serum Tears
Avoid Activities that Require Focus
Azasite (Azithromycin Ophthalmic)
Blephadex™
Blinking Exercises
Blink Reminder App
Botox and Hyaluronic Acid Gel Injections
Cevimeline (Evoxac®) and Pilocarpine (Salagen®)
Cliradex™
Cold Compresses or Ice
Contact Lenses that are Very Wet
Corticosteroid Drops and Ointments
Doxycycline, Minocycline
Eliminating Allergens
Eliminating Caffeine
Expressing Meibomian Glands
Eyelid Scrubs/Wipes/Cleansers
Glasses that Fog
Intraductal Meibomian Gland Probing
IPL (Intense Pulse Light)
Ivermectin, Oral
Ivermectin, Topical
LACRISERT Inserts
Lid Hygiene
Lid Margin Debridement
Lid Massage
Lipiflow®
Lubricating Eye Drops
Lubricating Ointments
MiBoFlo®
Moisture Chamber Goggles
Narrowing the Opening Between the Eye Lids
Omega 3 Fatty Acids
Oral Antihistamines
Other Important Nutrients
Pain Medications
Punctal Cautery
Punctal Plugs
Radio Waves and Thermal Cautery
Removing Lashes
RESTASIS®, IKERVIS (Cyclosporine)
Scleral Lenses
Sleeping
Sleep Mask
Stem Cell Therapy
Taping Eyes Closed
Treating Food Sensitivities
Trigger Reflexive Tears
Warm Compresses
Water and Hydration
Weights or Springs in Eye Lids
Wet Contact Lenses
Wrap-Around Glasses
Xiidra™ (Lifitegrast Ophthalmic Solution ) 5%
Treatments for Specific Diseases
General Treatment Recommendations
Treating Anterior Blepharitis
Treating Aqueous Deficiency
Treating Computer Vision Syndrome
Treating Conjunctivochalasis
Treating Epiphora
Treating Infections
Treating Inflammation
Treating Lagophthalmos
Treating Meibomian Gland Dysfunction (MGD) and Posterior Blepharitis
Treating Meibomian Gland Dysfunction (MGD) Caused by Demodex Mites
Treating Ocular Allergies
Other Ways to Improve Eye Comfort
Support Not A Dry Eye Foundation. When you shop at smile.amazon.com, Amazon donates 0.5% of your purchase.